Breast cancer care
Breast cancer is the most commonly diagnosed cancer among Australian women, with an estimated one in seven expected to hear those words in their lifetime. It’s a statistic that feels confronting — but behind it lies a powerful truth: outcomes have never been better with data showing that five-year survival for breast cancer has improved from 78 per cent to more than 90 per cent in recent decades. Earlier detection, advances in treatment and the strength of the communities that rally around those affected are important parts of the picture.
While the term “breast cancer” is often spoken in broad strokes, the reality is deeply individual. Each diagnosis carries its own biology, treatment path and emotional weight. For many women, the journey begins long before the first appointment, in moments of uncertainty, screening or self-checks. For others, it begins suddenly: a phone call, a biopsy result, an unexpected turn in life’s rhythm.
This special report aims to cut through confusion and fear with clarity and compassion. Together with leading Australian experts, we’ll explore what breast cancer is, how it’s detected, the risk factors and stages, the evolving treatment landscape and what it means to live well during and beyond the disease. Knowledge is power and, in the case of breast cancer, it can be lifesaving.
What is breast cancer?
Breast cancer is a disease in which abnormal cells in the breast grow in an uncontrolled way. Normally, the body’s cells grow, divide and die in a regulated cycle. Cancer develops when this process goes awry and the cells continue to grow and divide without order. These cells can form a lump (tumour), which may be benign (non-cancerous) or malignant (cancerous). Malignant tumours have the potential to invade surrounding tissue and spread to other parts of the body via the lymphatic system or bloodstream in a process known as metastasis.
Breast cancer can begin in different parts of the breast, most commonly in the ducts (ductal carcinoma) or lobules (lobular carcinoma), where milk is produced or carried. Some cancers remain localised (in situ), while others are invasive from the outset. The exact behaviour and growth rate can vary greatly from one cancer to another, which is why personalised diagnosis and treatment are so important.
While the words “breast cancer” can understandably provoke fear, it’s important to recognise that treatments continue to advance and survival rates have improved significantly. With the right combination of medical care, support and information, many women (and some men) diagnosed with breast cancer go on to live long, healthy and fulfilling lives.
Risk factors and prevention
Breast cancer is complex, with no single cause. It usually develops through a combination of factors, some over which we have degrees of control and others beyond it. Understanding these can help inform lifestyle choices and guide conversations with healthcare providers.
Unchangeable factors include being female (although men can develop breast cancer), increasing age and certain inherited gene mutations — most notably BRCA1 and BRCA2, which can significantly increase the lifetime risk of breast and ovarian cancers. A personal or strong family history of breast or ovarian cancer can also raise risk. Breast density, which refers to the amount of glandular tissue in the breast compared to fatty tissue, is another factor, as denser breasts can both increase risk and make detection more challenging.
Hormonal and reproductive factors also play a role. Early-onset menstruation, late menopause, not having children or having a first child later in life can slightly increase risk, likely due to prolonged exposure to oestrogen. Hormone replacement therapy (HRT), particularly combined oestrogen-progestogen therapy, has been linked with a small increase in breast cancer risk when used over several years.
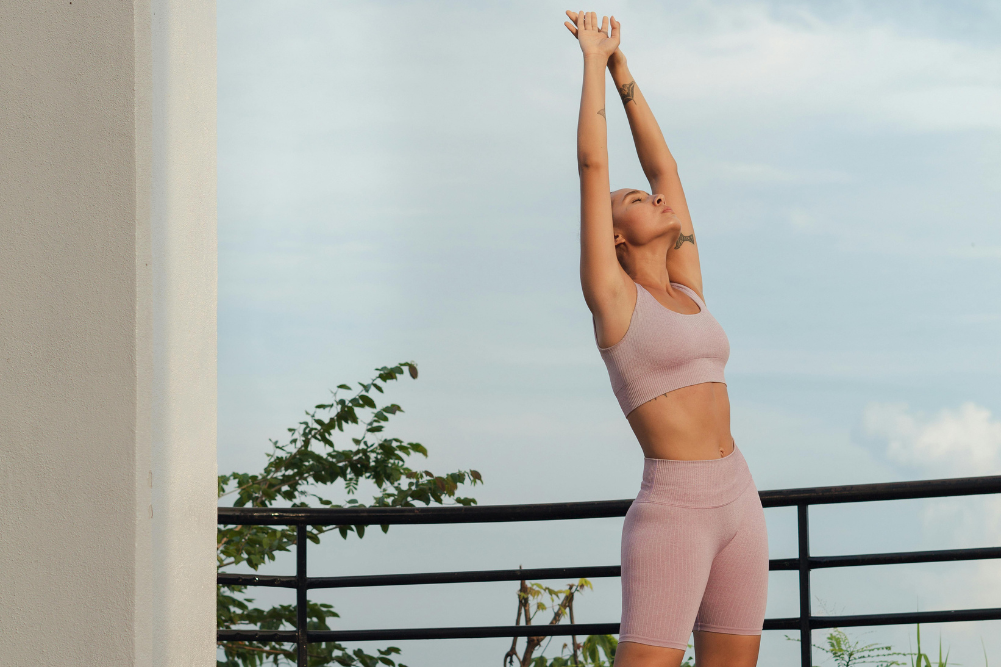
While no one can entirely prevent breast cancer, Professor Sherene Loi, senior medical oncologist and breast cancer research leader at Peter MacCallum Cancer Centre, says it is a common misconception that breast cancer risk cannot be modified because it is mostly genetic. “Regular physical activity can significantly reduce risk — even for women with a family history,” she advises, noting that current guidelines recommend at least 150 minutes of moderate-intensity aerobic exercise each week, along with regular resistance training, both “associated with lower risk of breast cancer and improved outcomes after diagnosis and treatment”.
In addition to regular exercise, evidence suggests certain lifestyle actions may lower risk. These include maintaining a healthy weight, limiting alcohol intake, avoiding smoking and eating a balanced diet rich in plant foods. Breastfeeding, if possible, is also associated with a modest reduction in risk.
Screening and early detection remain cornerstones of prevention strategies. Staying informed and proactive offers the best chance of catching any changes early.
Detection and diagnosis
There is a greater chance of successful treatment the earlier breast cancer is found. Regular screening, self-awareness and prompt investigation of any changes form the foundation of early detection and save lives.
Screening
“Screening is especially important as breast cancer risk increases with age,” says Loi, “even in women with no family history.” In Australia, the national screening program, BreastScreen Australia, offers free mammograms every two years for women aged 50–74, with invitations sent by mail.
Those at higher risk may need more frequent or earlier checks. Women aged 40–49 and over 74 can also access free screening, although they are not automatically invited. Mammography is currently the most widely used screening tool, able to detect many cancers before they can be felt.
For those at higher risk due to family history, genetic factors or previous breast cancer, additional imaging such as an ultrasound or magnetic resonance imaging (MRI) may be recommended. These tools can be particularly helpful in women with dense breast tissue, where mammograms can be less sensitive.
“If you’ve been told you have dense breasts, it is important you talk to your doctor about additional imaging — this is particularly relevant for younger women,” Loi advises, highlighting that as of mid-2025, a national policy now recommends BreastScreen services to inform women of their breast density. States including South Australia, Victoria, New South Wales and Western Australia already provide this in result letters, while other states are rolling it out. “Knowing your density supports more personalised risk discussions with your doctor,” she says.
Self-checks
While screening is crucial, it’s equally important to be familiar with how your breasts normally look and feel. Changes to watch for include:
- A lump or thickening in the breast or underarm
- Alteration in size, shape or contour of the breast
- Dimpling or puckering of the skin
- Nipple changes, such as inversion, discharge or redness
- Unexplained pain in the breast or armpit
If any of these symptoms appear, prompt medical assessment is essential. While most changes are not cancer, only further tests can confirm this, and it is always best to take swift action in investigating it.
Diagnostics
A breast cancer diagnosis typically involves a combination of clinical breast examination, imaging (mammogram, ultrasound or MRI) and biopsy. A biopsy, where a small sample of tissue is removed and examined under a microscope, is the only definitive way to confirm breast cancer.
Receiving a diagnosis can be an overwhelming experience. Support from healthcare providers, family and specialist cancer support organisations can make a difference during this time, helping patients navigate decisions about treatment and care.
Treatment options and emerging advances
No two breast cancer journeys are the same — and neither are treatment plans. The most effective approach is tailored to the individual, considering the type and stage of the cancer, tumour biology and personal factors such as age, general health and preferences. For many women, treatment involves a combination of therapies designed to remove or destroy the cancer, reduce the risk of recurrence and preserve quality of life.
Australians are fortunate when it comes to a unique strength of Australia’s healthcare system, which ensures treatment equity. “Our public health system provides free access to world-class breast cancer treatment and clinical trials, ensuring high-quality care regardless of income and insurance status to Australian residents,” Loi shares. This level of access is rare globally and underpins the country’s commitment to equitable care.
Standard treatment options can include surgery, radiation therapy, chemotherapy, hormone therapy, targeted therapy and, increasingly, immunotherapy. The choice and sequence of these treatments depend on a range of clinical factors, as well as the patient’s individual goals and circumstances.
- Surgery may involve breast-conserving surgery (lumpectomy) or mastectomy, depending on tumour size, location and personal preference. Lymph nodes are often assessed to check for spread.
- Radiation therapy uses high-energy X-rays to destroy residual cancer cells post-surgery. Modern techniques increase precision and reduce impact on surrounding tissue.
- Systemic therapies travel through the bloodstream to target cancer cells throughout the body:
- Chemotherapy kills or slows cancer cell growth, used before surgery (neoadjuvant) to shrink tumours or after surgery (adjuvant) to reduce recurrence risk.
- Hormone therapy blocks or lowers oestrogen in hormone receptor-positive cancers.
- Targeted therapy focuses on specific molecular changes, such as HER2-positive tumours.
- Immunotherapy mobilises the immune system to attack cancer cells.
According to Loi, advances in technology and pharmacology have resulted in some newer medications, such as immunotherapy and antibody–drug conjugates “reshaping treatment for even the most aggressive breast cancers” and providing options with “greater precision and fewer side effects”.
Treatment options and emerging advances
The progress in personalised medicine has also transformed breast cancer care, tailoring treatment to the unique genetic and molecular features of each tumour. As Loi explains, “This has resulted in some types of breast cancer becoming highly curable if detected early enough. Advances in genome sequencing and molecular profiling now allow us to identify the drivers of each cancer more precisely, improving outcomes while sparing patients from unnecessary toxicity.”
Alongside these treatment breakthroughs, genetic testing is becoming more widely available, enabling clinicians to better identify inherited risk and create targeted prevention or early detection strategies. This not only benefits women diagnosed with breast cancer, but also their families, by helping guide screening and proactive care before cancer develops.
From a personalised treatment outlook, while the goal is always to eliminate cancer, equal attention is given to preserving a woman’s sense of self, physical function and long-term wellbeing. For many, a multidisciplinary team — including surgeons, oncologists, nurses, physiotherapists and psychologists — ensures that care is not only effective, but holistic.
Living well during and beyond treatment
The experience of breast cancer and its treatment affect more than just the body — it can touch every part of life. Fatigue, changes in appearance and emotional highs and lows are common. However, with the right strategies and support, many women find ways to live well throughout treatment and into survivorship.
Supporting physical wellbeing
During treatment, energy levels may fluctuate. Gentle, regular movement such as walking, stretching or yoga can help maintain strength, improve mood and ease side effects like fatigue and stiffness. Accredited exercise physiologists with cancer expertise can tailor safe programs for each stage of treatment. Good nutrition is also essential, focusing on whole foods, adequate protein and hydration to help the body repair and recover.
Rest is equally important. Listening to the body’s cues and pacing activities can help prevent burnout. Managing side effects such as nausea, pain or lymphoedema with the guidance of a healthcare team can also make daily life more comfortable.
Caring for emotional health
A breast cancer diagnosis can stir feelings of fear, sadness or uncertainty. Psychologists, counsellors and support groups provide a safe space to process these emotions and share experiences with others who understand. Mindfulness, meditation and breathing exercises can help calm anxiety and improve resilience.
Professor Phyllis Butow, a clinical psychologist and psycho-oncology researcher at The University of Sydney’s School of Psychology, notes that life after active treatment often brings its own challenges. There can be an expectation to return to “normal”, but survivors may find themselves facing ongoing fears of recurrence, particularly at follow-up appointments or when new symptoms appear. “Many women lose confidence in their body to stay well, even those told their chances of cure are high. These worries may ease over time but, for some, they remain ever-present,” she says. Ongoing side effects — from instant menopause to fatigue — can affect self-image, energy and daily life.
Body image and self-confidence
Changes to appearance, ranging from hair loss and surgical scars to weight fluctuations, can be confronting. Some women find confidence in exploring wigs, headscarves or specialist lingerie designed for post-surgery comfort. Others embrace their appearance as a reflection of their strength and survival. If you’re navigating this, reconnecting with activities and styles that make you feel most like yourself can be an important step in restoring self-esteem.
Professor Butow adds that altered appearance and physical changes may affect feelings of femininity and desirability, particularly for women who have had part or all of a breast removed or their ovaries taken out. “These can take away confidence, challenge a woman’s sense of self and require accommodation in daily life and work,” she says. Addressing these feelings openly — with a partner, healthcare professional or peer support group — can be key to rebuilding one’s confidence and self-connection.
The role of social support
Family, friends and community networks play a vital role in emotional wellbeing. Accepting offers of help — whether it’s a meal, a lift to appointments or simply company — can lighten the load. Cancer support organisations offer services ranging from peer mentors to practical assistance with transport and home care.
If you’re navigating breast cancer, your loved ones often want to help but may not know how. Be specific about your needs and remember that accepting help is not a sign of weakness. It’s a way of conserving your energy for healing.
Support from peers who have been through a similar experience can be particularly valuable. Butow highlights the benefits of structured programs such as one-on-one peer support, cancer support groups and free online tools such as Finding My Way. These, along with professional help from skilled nurses, social workers, psychologists or helplines “can lift the burden from women’s shoulders as they adjust to life after breast cancer”, she says.
Life beyond treatment
When active treatment ends, many women feel relief yet also riddled with uncertainty. Follow-up appointments, ongoing medication or lingering side effects can be a reminder that life has changed. Establishing a wellness plan with your healthcare team can provide structure and reassurance, incorporating regular check-ups, healthy lifestyle habits and strategies to manage late effects of treatment.
Thriving after breast cancer often means finding a “new normal” — a life shaped by the experience but not defined by it. Many survivors speak of a renewed appreciation for health and self-care, deeper connections and a clearer sense of priorities. Every journey is unique, and so is every recovery.
Looking forward
By combining medical expertise, early detection, emotional and physical support, and the courage of those affected, we continue to see progress in both survival rates and quality of life after breast cancer.
If you or someone you know has been diagnosed, remember that help is available and hope is real. Knowledge empowers, support strengthens and the path ahead, while incredibly challenging, can still hold moments of joy, connection and renewal.
Support and resources
A breast cancer diagnosis can feel isolating, but no one has to face it alone. Across Australia, there is a strong network of organisations, healthcare professionals and community groups dedicated to providing information, emotional support and practical assistance at every stage of the journey.
Support services
Cancer Council (13 11 20) offers a free, confidential telephone information and support line, along with local programs, peer groups and online forums.
Breast Cancer Network Australia (BCNA) connects people affected by breast cancer with resources, advocacy and support from those who have walked the same path.
McGrath Foundation funds specialist breast care nurses who provide free support from diagnosis through treatment and beyond.
Lifeline (13 11 14) offers 24/7 crisis support for anyone experiencing emotional distress.
Your treating hospital or cancer centre may also have social workers, psychologists, dietitians and exercise physiologists available as part of your care team. Asking your GP or oncologist for referrals can help you access these services.