Thriving In Perimenopause
Perimenopause impacts mind, body, and skin—awareness and self-care can make this transition easier and more empowering.
Perimenopause marks the transitional phase leading up to a woman’s final menstrual period, often beginning as early as the late 30s and extending into the mid 50s. During this time, levels of oestrogen and progesterone fluctuate significantly, affecting nearly every system in the body. Despite being a natural part of the ageing process, perimenopause remains under‑recognised and often misunderstood. The lack of conversation and awareness around this transition leaves many women feeling unprepared, isolated and unsure of how to navigate the physical and emotional shifts it brings. With up to 60 per cent of women experiencing mild to moderate symptoms and 20 per cent facing symptoms severe enough to impact their daily lives, it’s concerning that the discourse around this inevitable phase of a woman’s life isn’t more widespread.
Fortunately, while the symptoms of perimenopause can be broad and deeply impactful, this phase does not have to be marked by confusion or suffering. With the right education, support and open conversation, women can feel informed, supported and empowered throughout their journey.
Symptoms
Perimenopause typically spans four to six years but can last anywhere from one to 10. During this time, fluctuations in key hormones including oestrogen, progesterone, follicle‑stimulating hormone (FSH) and androgens such as testosterone are common. The ovaries’ responsiveness to hormonal signals from the brain naturally declines, which impacts both egg quality and ovulation frequency. These hormonal fluctuations can trigger a cascade of symptoms, with more than 70 identified. Some of the most common include:
- Irregular or heavy periods
- Hot flushes and night sweats
- Fatigue, sleep disturbances
- Anxiety, mood swings, depression
- Brain fog and forgetfulness
- Vaginal dryness, decreased libido
- Weight changes, muscle loss, reduced bone density
- Skin changes
Menstrual cycle changes
One common early sign of perimenopause is a shift in a woman’s menstrual cycle. Fluctuating levels of key hormones such as oestrogen, progesterone, follicle stimulating hormone (FSH) and testosterone can lead to longer or shorter cycles, or even skipped periods. As ovulation becomes more irregular, fertility naturally begins to decline. For many women, especially those who have had “clockwork” cycles throughout their lives, this change can feel confusing and even distressing.
The uterus also undergoes changes during this time. Alterations in the endometrial lining may lead to heavier or more irregular bleeding patterns, while declining oestrogen impacts the health of vaginal and vulval tissues. The vaginal walls may become thinner, drier and less elastic, and the vaginal pH tends to shift toward a more alkaline state. These changes can cause vaginal dryness, irritation, burning or discomfort during sex, and can increase susceptibility to infections such as UTIs, thrush and bacterial vaginosis.
While these reproductive changes may initially sound a little disheartening, the good news is that many of these symptoms can be supported effectively with natural approaches. A simple hormonal blood test can offer valuable insight into your current hormonal picture. Once you have a clear understanding of which hormones are shifting, you and your health care professional can develop a targeted plan that combines nutritional support and key lifestyle changes to mitigate or ease any challenges.
Herbal medicine may also offer gentle, effective support. Herbs commonly used to support oestrogen, FSH and testosterone balance are chaste tree, shatavari, wild yam and tribulus. Nervine and adaptogenic herbs such as lemon balm, withania (ashwagandha) and rhodiola may help nourish the nervous system and support overall resilience. Always consult a naturopath to tailor a regimen for your unique needs.
Metabolic changes
Many women are surprised when their usual routines for maintaining weight and energy levels stop working. Lara Briden, a naturopathic doctor and bestselling author with more than 30 years of experience in women’s health, refers to this as a “major metabolic upheaval”, a time when the body’s relationship with energy, hunger and fat storage changes dramatically. “First, progesterone drops and then oestrogen. This hormonal decline contributes to increased insulin resistance, reduced cellular energy and a shift in fat storage toward the abdomen,” Briden explains. “Oestrogen is a metabolic superstar. It supports insulin sensitivity, increases energy expenditure and helps build muscle. It even reduces hunger.”
Meanwhile, progesterone has a more nuanced role. While it can increase appetite and decrease insulin sensitivity, it also calms the nervous system, lowers inflammation and can help moderate excess testosterone, another contributor to abdominal weight gain in women. Importantly, Briden notes that synthetic progestins (as found in birth‑control pills) do not confer these benefits.
Oestrogen and progesterone also interact with other key metabolic regulators: thyroid hormones, cortisol and gut-derived hormones like GLP‑1. Notably, perimenopause is a time when conditions such as Hashimoto’s thyroiditis commonly emerge, particularly for those who previously experienced postpartum thyroid issues. Briden highlights the influence of the nervous system and how it responds to stress, too. “A healthy oscillation between sympathetic and parasympathetic states supports insulin sensitivity and metabolic flexibility.” If you’re living in a chronic “fight‑or‑flight” state, it will directly impact how your body metabolises food and stores fat.
In her book The Metabolism Reset, Briden outlines a holistic plan to support women through these changes. She shares some key foundational strategies:
- Prioritise nourishment: Focus on whole foods, home-cooked meals, quality animal proteins and micronutrients. Briden especially recommends magnesium and inositol.
- Regular movement: Build muscle and regulate the nervous system with strength training and outdoor activity that supports circadian rhythm.
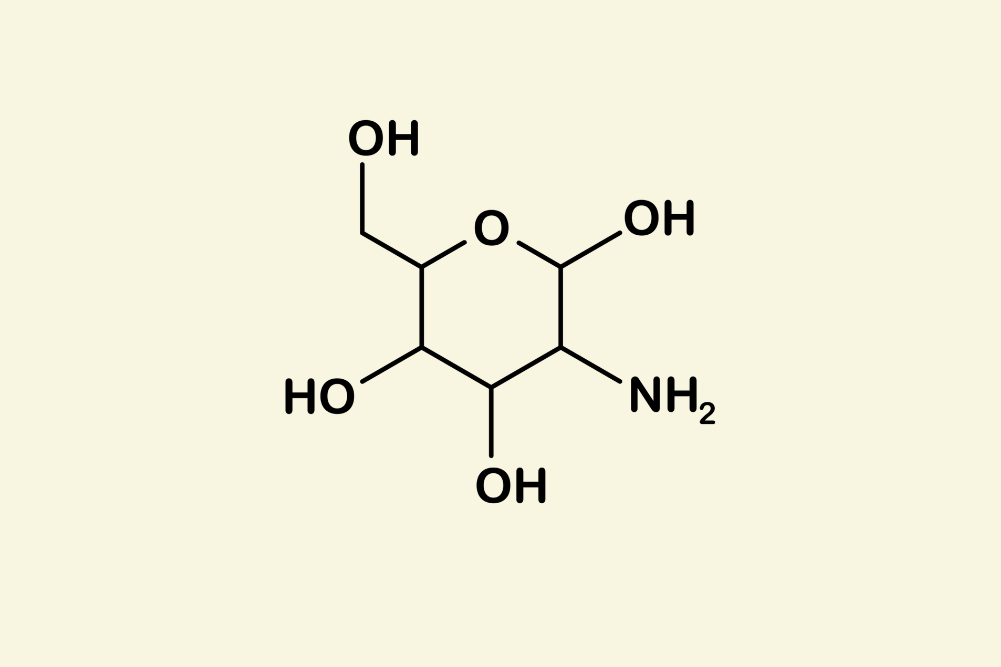
- Address gut health: Gut inflammation can drive insulin resistance and weight gain.
- Limit ultra-processed foods (namely sugar and refined carbohydrates) and alcohol: These can exacerbate metabolic dysfunction and worsen symptoms like night sweats.
- Boost connection: Social interaction can elevate oxytocin, an important metabolic and mood-regulating hormone.
Beyond merely surviving
Thriving in perimenopause, according to Briden, is about working with the body, not against it. When you recognise metabolic changes early and adapt accordingly, there is so much that can be done to manage these symptoms. “Women who thrive are usually the ones who enter this phase with good gut health, are not on weight‑promoting medications like hormonal birth control, eat a mostly whole-food diet and have a regular movement practice they enjoy,” Briden says. “Those who struggle often carry unresolved health issues or rely on traditional weight-loss advice like calorie counting.”
Michelle Bridges, renowned Australian personal trainer and creator of The Perimenopause Method, knows the challenges of perimenopause firsthand. During the COVID‑19 lockdown, while researching her program The Menopause Method, she began experiencing puzzling symptoms: poor sleep, a painful hip, tinnitus, anxiety and a persistent emotional flatness. “I tried to explain it away,” she recalls. “I thought it was the pandemic or being a single parent, but something just didn’t feel right.”
Her GP offered antidepressants, but Bridges chose not to fill the prescription. Instead, she continued researching and soon recognised that she was in perimenopause. The experience was eye‑opening. “This whole space was like an iceberg, there is so much more below the surface. Women need this education because we’ve been left out of the conversation. Understanding what’s happening in your body means you can make informed choices.”
Drawing on her expertise in fitness, Bridges leaned into movement as a tool for balance. And she’s quick to emphasise that exercise is not just a “nice to have”, it’s essential for this phase of life. “Strength training is the best bang for your buck,” she says. “Heavy weights build muscle and protect bone density. Jump training, like hopping, skipping or sprinting helps bone strength, especially in the hips. And cardio bursts, even five minutes of sprints after your session, can help shift stubborn weight and lift your mood.”
Education and boundaries
Bridges is also passionate about highlighting how brain health is affected during this transition. The brain is rich in oestrogen receptors, and when levels drop, women can experience cognitive changes, emotional sensitivity and disrupted sleep. “You suddenly feel like your resilience has evaporated,” she says. “And because no one talks about perimenopause starting in your 30s or early 40s, most women don’t even realise what’s happening. Without the right help, it can be a lonely and scary experience.”
It’s important to also acknowledge that hormonal fluctuations, particularly the drop in oestrogen and changes in cortisol regulation, can significantly impact energy levels and motivation. These shifts can make it harder to find the drive to make changes to exercise, nutrition or self‑care, even when you know it would help. Understanding that this lack of drive is physiological, not just psychological, is the first step in finding more compassionate, sustainable ways to support yourself through it.
Bridges insists that education and boundaries are everything. “Perimenopause is not a jail sentence. You won’t become invisible. This is actually a time of empowerment, when you get to choose the direction of the next phase of your life. But you have to put yourself first.”
Bridges shares several key takeaways that have been shown to ease perimenopausal symptoms and enhance quality of life. Many of these align with Briden’s evidence-based recommendations:
- Learn to say no.
- Clean up your sleep hygiene (this might be the number‑one priority!).
- Get clear on who and what truly matters to you.
- Prioritise your own needs without guilt.
- Practise meditation or mindfulness.
- Stay connected with friends and family.
- Make regular movement a non‑negotiable, especially strength training, even if it’s just a weighted walk.
- Focus on nourishing, whole-food nutrition.
- Minimise or eliminate alcohol.
- Explore hormone replacement therapy (HRT) if it feels like the right fit for you.
- Don’t underestimate the power of therapy. It can be a true game-changer.
Intimacy and desire
Fluctuating sex hormones can also influence sexual desire. While some women experience a dip in libido, others notice changes in arousal or orgasm, which is influenced by both hormonal shifts and the emotional landscape of this season of life.
For vaginal dryness, topical coconut oil can be a gentle and effective natural lubricant and its antibacterial properties also help support a healthy vaginal microbiome.
Intercourse should not be painful, and open communication with your partner about the changes your body is experiencing is essential. Bridges says, “When these conversations come from a place of love, they can often bring you closer. Sex — good sex — doesn’t just happen on its own. Like with exercise, it takes work. Be consistent, or at least make an effort to move in the right direction. You might find that what you enjoy now is different from what you enjoyed 15 years ago, and that’s okay! Explore new things and bring curiosity into the bedroom.”
Skin changes
Another visible sign of hormonal changes during perimenopause often shows up on the skin. As oestrogen levels decline, the skin can become drier, thinner, more sensitive and prone to breakouts, pigmentation and flare-ups of pre-existing conditions. Skincare pioneer and MUKTI Organics founder, Mukti, who has spent decades at the forefront of the natural beauty industry, explains that women can lose up to 30 per cent of their skin’s collagen in the first five years after menopause. This contributes to reduced elasticity, increased dryness and more pronounced fine lines and wrinkles, largely due to slower cell turnover and diminished collagen production.
“As women enter perimenopause, it’s crucial to reassess and adapt skincare routines,” says Mukti. “This stage of life often calls for a complete overhaul to meet the skin’s evolving needs.” She emphasises the importance of early intervention with targeted skincare to help mitigate the effects of hormonal ageing, including premature signs of ageing.
Some of the key strategies Mukti has seen work effectively over the years include incorporating more hydrating and nourishing products, daily sun protection and the introduction of active ingredients that support skin health. “Vitamin C is brilliant for collagen production and brightness, niacinamide helps even out skin tone, and retinal increases cell turnover,” she notes.
When it comes to caring for your skin during this season of life, Mukti recommends focusing on gentle, nourishing steps that support hydration and barrier repair. Use a gentle cleanser to remove makeup and impurities without stripping away natural oils. A hydrating mist can help to refresh the skin and keep it hydrated throughout the day. A targeted serum with adaptogenic botanicals and restorative ingredients may help strengthen the skin’s defences and restore resilience. Lock in moisture and enhance smoothness with a hydrating oil. A protective daily moisturiser shields the skin from environmental stressors. At night, indulge in a rich, replenishing cream designed to restore the skin’s lipid barrier and support overnight repair.
She also reminds women not to overlook the rest of the body. “There’s a misconception that body skin doesn’t need the same level of care as facial skin, but it’s often the first to show signs of ageing,” she explains. Look for products that are specifically formulated to reduce redness, soothe irritation and smooth uneven skin tone. It’s important they are designed to calm reactive skin and strengthen the barrier while offering a carefully balanced blend of healing antioxidants, lipids and skin-repairing actives. Mukti notes that many women benefit from formulations like these that not only treat visible signs of ageing but also support deeper skin health over time.
Mukti takes a holistic view of skin health, believing that what appears on the surface often reflects internal shifts. Echoing the advice shared by Briden and Bridges, she says: “Skin is our largest organ, and it’s often a mirror of our emotional and hormonal state. Supporting it requires more than just good products, it’s also about what you’re eating, how well you’re sleeping and the stress you’re carrying.” A diet rich in antioxidants and omega‑3 fatty acids, good sleep hygiene and emotional balance are, she adds, essential parts of the skincare conversation.
Nurturing yourself
Caring for your whole self becomes more important than ever during perimenopause. Nourishing yourself with nutrient‑dense food, consistent movement, quality rest and open, supportive conversations can go a long way in promoting hormonal balance, physical vitality and emotional resilience. Regularly tuning in to your body and recognising when something feels off is key, and seeking help early can make all the difference.
When approached with curiosity, kindness and inspired action, perimenopause becomes a powerful invitation to step into the next, evolved version of yourself and a new chapter of life, where who knows what magic awaits.